
AMR: The Fact Sheet

AMR: The Fact Sheet
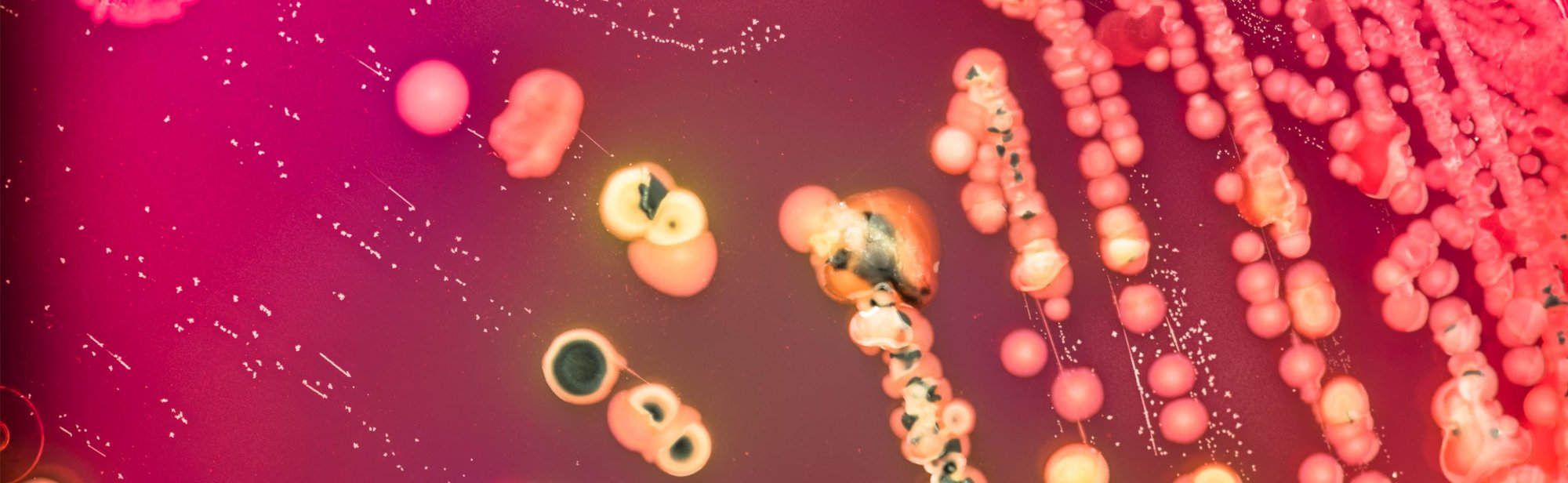
Antimicrobial Resistance is when existing microbials become less effective due to baceteria adapting and becoming resistant to medicine.1
If you're hearing about AMR for the first time, we want to start off by letting you know that the World Health Organisation has declared that Antimicrobial Resistance is one of the top 10 global public health threats facing humanity.
AMR was, directly and indirectly, responsible for an estimated five million deaths in 2019. By 2050, up to 10 million deaths could occur annually - matching the 2020 rate of cancer deaths. Put into context, AMR could kill more people than cancer - a pretty alarming statistic!
If not dealt with, AMR could shave off $3.4 million off Global Domestic Product (GDP) annually and push 24 million people into extreme poverty in the next decade.
It's safe to say we're facing a pretty big threat, and we all need to play our part to help prevent this from becoming our reality.
What is Antimicrobial Resistance?
Antimicrobial resistance (AMR) occurs when bacteria, viruses, fungi, and parasites change over time and no longer respond to medicines making infections harder to treat and increasing the risk of disease spread, severe illness, and death.
As a result of drug resistance, antibiotics and other antimicrobial medicines become ineffective and infections become increasingly or impossible to treat.
What are antimicrobials?
Antimicrobials, including antibiotics, antivirals, antifungals, and antiparasitics, are used to prevent and treat infections in humans, animals, and plants.

Why is Antimicrobial Resistance a global concern?
The emergence and spread of drug-resistant pathogens have acquired new resistance mechanisms, leading antimicrobial resistance, continues to threaten our ability to treat common infections. Especially alarming is the rapid global spread of "superbugs" that cause infections that are not treatable with existing microbial medicines such as antibiotics.
The clinical pipeline of new antimicrobials is dry. In 2019, WHO identified 32 antibiotics in clinical development that address the WHO list of priority pathogens, of which only six were classified as innovative. Furthermore, a lack of access to quality antimicrobials remains a major issue. Antibiotic shortages are becoming increasingly ineffective as drug-resistance spreads globally leading to more difficult to treat infections and deaths. New antibacterials are urgently needed.
What accerelates the emergence and spread of antimicrobial resistance?
AMR occurs naturally over time, usually through genetic changes. Antimicrobial resistant organisms are found in people, animals, food, and the environment (in water, soil, and air). They can spread from person to person or between people and animals, including from food of animal origin. The main drivers of antimicrobial resistance include the misuse and overuse of antimicrobials; lack of access to clean water, sanitation and hygiene (WASH) for both humans and animals; poor infection and disease prevention and control in healthcare facilities and farms; poor access to quality, affordable medicines, vaccines, and diagnostics; lack of awareness and knowledge; and lack of enforcement of legislation.
What are world leaders doing to tackle AMR?
Governments all over the world have created National Action Plans that set out specific actions that will help combat AMR. You can find the UK's 5 year national action plan here.
In addition to the National Action Plans, leading organisations all over the world are developing guidance and support the enables the world to prepare for the realities of AMR, a great example being the World Health Organisations core package of interventions to support national action plans, which can be viewed here.
What three things can be done as individuals to prevent AMR from becoming a global threat?
- Good hand hygiene: Wash your hands regularly to prevent infections, avoid getting sick and keep from spreading germs. Also, wash your hands after touching, feeding, or caring for animals.
- Use antimicrobials only when needed and prescribed for by your healthcare professional. Remember that most upper respiratory infections, such as cold and bronchitis, do not require treatment with antimicrbials.
- Prepare food safely to avoid foodborne infections and ensure homes, offices, and work areas are regularly cleaned and disinfected to ensure micro-organisms are not harbouring on surfaces and touch points.



How can Vernacare help in the fight against AMR?
As we mentioned earlier, the World Health Organisation has created a core package of interventions to support the national action plans and the first pillar within this core package is...Infection Prevention.
All of our products here at Vernacare are designed to prevent the spread of infections, it's quite literally what we do. We have a wide range of solutions that help to prevent the spread of infection across a number of different healthcare facilities.
Our Infection Prevention Solutions
- Our Azo™ range of cleaning and disinfection solutions have been designed to kill micro-organisms on surfaces and non-invasive medical devices in as little as 15 seconds.
- Newly available on the market, our gentle range of Conti® Wet and Dry Wipes are designed to support individualised care routines, and provide a clear alternative to traditional soap and water bathing, and eliminate the associated infection risks.


- For decades, we've led the way with Vernacare's single-use, disposable medical pulp which is now widely adopted across the NHS and globally. The benefits of using single-use medical pulp as opposed to a reusable plastic bed pans is clear to see, with studies highlighting increased infections where reusable bedpans are used.
- Combining our single-use medical pulp with our newest macerator, the Vortex Air, provides an alternative to manual bedpan washing and disinfecting, and a quicker, safer solution for healthcare professionals.


- Clinical Waste Management is a key area where if done incorrectly, it can lead to devastating consequences including infection outbreaks, sharps injuries, and lifelong issues for those involved. Our Sharpsafe and Clinisafe waste management products are designed to provide the optimal solutions for all Clinical Waste Management needs with easily-identifiable colour-coded products, safety shields and temporary closures, plus they are made from up to 100% recycled materials.
- Single-use instruments are key to preventing infections, and our range of Instrapac® instruments and procedure packs are designed to break the chain of infection, with immediate disposal after each use. Arriving in sterile packaging and ready for use, they take away a need for costly and potentially risk resterilisation processes, and provide peace of mind that each instrument is sterile and safe to use, every time.


One final thing...the impact of Global Warming, Zoonosis, and infection risks.
Zoonotic diseases are at the nexus of climcate change, changes in ecosystems, and human health. Zoonotic diseases, or zoonoses, are classically defined as diseases and infections that are naturally transmitted between veterbrate animals and humans.
According to the annual publication of The Lancet Countdown on human health and climate change from October 2022, there is a 48% chance that the 1-5°C threshold decided in the Paris Agreement will be exceeded within 5 years. This will impact on all forms of zoonoses be it water, food, vector, rodent, or airbourne origin and will also increase the emergence of novel infections with pandemic potential.
The climate suitability for vectorbourne diseases, such as dengue and malaria, is changing, as witnessed by a 12% increase in dengue's transmission between 1951-60 and 2012-2021, and in the case of malaria with a possibility of it reappearing in southern Europe due to increased geographical range
In summary, this means that as climate change worsens, animals will move more mainland and diseases will spread between animals and humans. If you add AMR into this reality, where antibiotics no longer work, the future looks like a scary place.
In the face of this grim picture, there are rays of hope, such as the increased individual commitment to mitigate climate change, increased media coverage, and the engagement of policymakers at high level meetings.
Here at Vernacare, sustainability is at the heart of everything we do. We know that we must reduce our environmental impact and create more sustainable solutions for the future. It's important that we keep these realities in our minds as we speak to our team members, and our customers. We should be asking ourselves, "how can we be more sustainable?", "what can I do to reduce my environmental impact?". Let's ask our customers and partners about their plans and priorities to ensure we're all working towards a more sustainable future.
Get in touch with us today to learn how our solutions can support in the fight against AMR
Contact Us