
The impact of sharps injuries

The impact of sharps injuries
Sharps injuries are one of the most common work-related injuries faced by healthcare workers, with the potential injuries carrying a huge amount of risk.1
Over 60 pathogens can be transferred via a needlestick injury2, and recent studies have shown there can be a massive burden to mental health due to the extensive checks needed to identify if the healthcare worker has contracted a bloodborne virus due to an injury.
We will outline what a sharps injury is, the risks they pose to healthcare workers, and how the risks can be minimised through a robust sharps management system, including proper use and disposal.
What is a sharps injury?
A sharps injury is an incident which causes a needle, blade (such as a scalpel), or other medical instruments to penetrate the skin. This is sometimes called a percutaneous injury.
Items that can cause sharps injuries include:
- Blood collection needles
- Bone fragments or teeth
- Broken glass
- Emergency services cutting equipment
- Instruments used in invasive operations, surgery, dentistry, and acupuncture
- IV cannulas or needles used to connect parts of the IV delivery systems
- Jagged metal
- Lancets
- Needles such as hypodermic and hollow bore
- Razors
- Scalpels
- Scissors
- Winged steel needles, known as butterfly needles
- Other necessary medical instruments
With such an extensive list of possible causes, it is impossible to remove the usage of sharps completely from healthcare workers day to day roles. As per health and safety regulations, wherever possible the use of safe sharps is always encouraged4, however the disposal of safer sharps needs to be taken with the same level of care as normal sharps.
What are the risks of needlestick injuries?
Since 1979, our Sharpsafe team have engineered purpose designed products with the aim of minimising the risks of needlestick and sharps injuries. Needlestick injuries are the most common occupational hazard among healthcare workers and are all preventable through proper training and procedures.
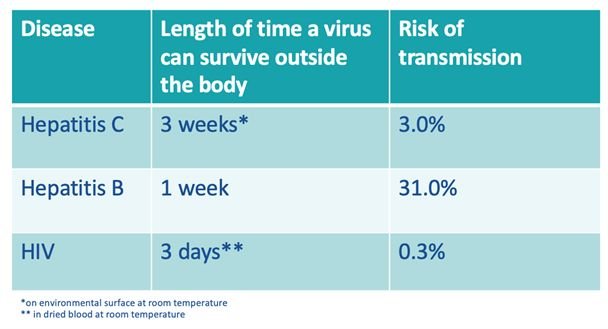
These injuries carry a risk of the transmission of bloodborne viruses such as Hepatitis C, Hepatitis B, and HIV; lifelong conditions that impact the health of patients and staff, and costs the NHS and healthcare facilities valuable time, resource, and money.
Based on data from a Royal College of Nursing survey of 7,571 nurses in 2020, six out of ten nurses have experience a needlestick injury during their careers.5 However, the issue is one that solely impacts the nursing community. According to the World Health Organisation, more than two million sharps injuries occur annually among 35 million healthcare workers6, and 94% of practicing UK surgeons have been personally affected by a needlestick injury, or have seen a colleague experience one.7
Mental Health concerns
After the risk of bloodborne viruses, the second longest lasting side effect of a sharps injury is the mental burden they can carry. The wait for the 'all clear' from an injury can be up to six months. Within this time, those that suffered injuries have reported suffering anxiety, stress, depression, and even Post Traumatic Stress Disorder.10
More research is taking place to determine the mental health issues associated with sharps injuries, and particularly needlestick injuries. This research has indicated that 37% of nurses who have experienced a needlestick injury show evidence of PTSD for up to two years after the injury.11 The issues expanded into populations of doctors with 12% of those who have experienced a needlestick injury displaying at least one sign of PTSD post injury.12 Common feelings that emerge after experiencing such an injury include isolation, embarrassment, and anxiety.
The risk of bloodborne viruses
Bloodborne viruses are one of the biggest risks from sharps injuries. As the table shows, bloodborne viruses can survive for a considerable amount of time outside of the body. Hepatitis C can survive for up to three weeks outside the body, whereas Hepatitis B may only survive for one week but it does carry a 31% risk of transmission should a sharps injury occur.8
Although the risk of transmission is relatively low, it should be taken seriously. Sharps injuries need to be reported as soon as possible so that incident reports can be completed, and proper treatment determined. Ideally, a post-exposure prophlyaxis (PEP) for HIV ideally needs to take place within the first 72 hours of a sharps injury9 and any delay in reporting could result in life changing consequences.
Mitigating the risk
With one third of sharps injuries taking place during the disposal12 it is imperative in the fight to minimise sharps injuries that you employ a robust sharps management system. Sharpsafe have a comprehensive range of containers and accessories all of which are purpose designed and highly engineered for lowering the risk of injury.
Innovative and industry defining features such as incorporating the mandatory low dead space into the design of the lid, or the additional safety shield that prevents hands from touching anything below the fill have prevented sharps injuries since 1979.

Boost your knowledge with our new course
Our Key Account Managers are experts in developing a package that will suit the need of your facility, from the containers that you will require to, to the Near Patient Sharps Disposal accessories you will need to minimise the risks. They even provide full training during your product rollout and advice and product rationalisation during our annual sharps audits. All our customers now have access to a free CPD-certified sharps injury prevention course via the Vernacare Academy, giving a comprehensive overview into the risks of sharps injuries and how to minimise them.
There's never been a better time to join the Sharpsafe evolution. Contact us today to learn more and help minimise your facilities sharps injuries.
References
1 – www.nao.org.uk/publications/nao_reports/02-03/0203623.pdf
4 – https://www.legislation.gov.uk/uksi/2013/645/pdfs/uksi_20130645_en.pdf